This article is part of our continuing Fast Forward series, which examines technological, economic, social and cultural shifts that happen as businesses evolve.
As shortages of personal protective equipment persist during the coronavirus pandemic, 3-D printing has helped to alleviate some of the gaps. But Anthony Atala, the director of the Wake Forest Institute for Regenerative Medicine, and his team are using the process in a more innovative way: creating tiny replicas of human organs — some as small as a pinhead — to test drugs to fight Covid-19.
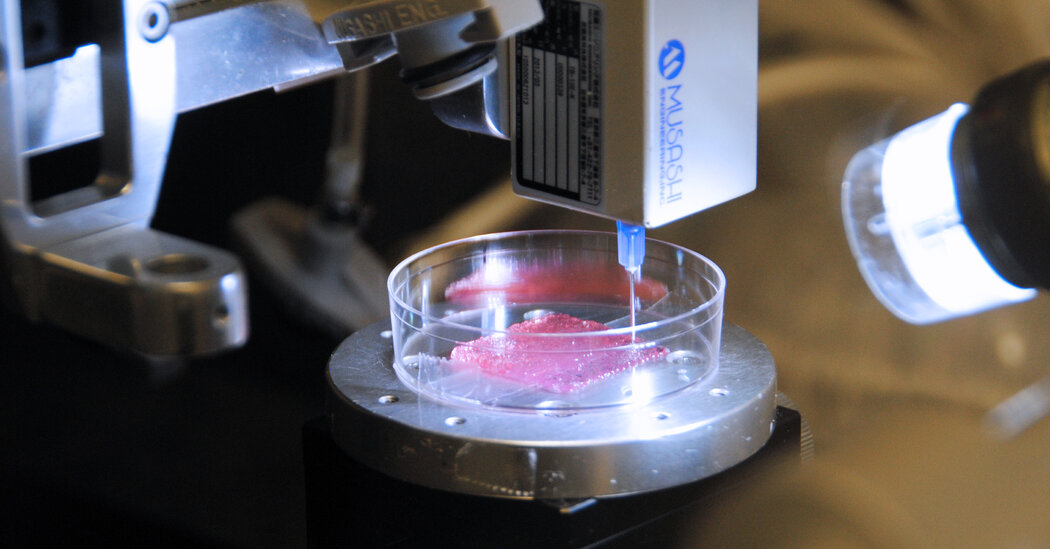
The team is constructing miniature lungs and colons — two organs particularly affected by the coronavirus — then sending them overnight by courier for testing at a biosafety lab at George Mason University in Fairfax, Va. While they initially created some of the so-called organoids by hand using a pipette, they are beginning to print these at scale for research as the pandemic continues to surge.
In the past few years, Dr. Atala’s institute had already printed these tiny clusters of cells to test drug efficacy against bacteria and infectious diseases like the Zika virus, “but we never thought we’d be considering this for a pandemic,” he said. His team has the ability to print “thousands an hour,” he said from his lab in Winston-Salem, N.C.
The process of constructing human tissue this way is a form of bioprinting. While its use in humans is still years away, researchers are honing the methods to test drugs and, eventually, to create skin and full-size organs for transplanting. Researchers are making strides in printing skin, critical for burn victims; managing diseases like diabetes where wound healing is difficult; and for the testing of cosmetics without harming animals, or, of course, humans.
“Even to us it sometimes seems like science fiction,” said Akhilesh Gaharwar, who directs a cross-disciplinary lab in the biomedical engineering department at Texas A&M University that focuses on bioprinting and other approaches to regenerative medicine.
Bioprinting’s importance for pharmaceutical analysis is paramount now, not only for potential Covid-19 treatments, but also for testing treatments for cancer and other diseases. Dr. Atala says that the organoids allow researchers to analyze a drug’s impact on an organ “without the noise” of an individual’s metabolism.
He cited Rezulin, a popular diabetes drug recalled in 2000 after there was evidence of liver failure. His lab tested an archived version of the drug, and Dr. Atala said that within two weeks, the liver toxicity became apparent. What accounts for the difference? An organoid replicates an organ in its purest form and offers data points that might not occur in clinical trials, he said, adding that the testing is additive to, rather than in lieu of, clinical trials.
Testing on bioprinted skin or other miniature organs also can more readily determine which drugs that work in animals like rats might not perform well in people.
“The 3-D models can circumvent animal testing and make the pathway stronger from the lab to the clinic,” Dr. Gaharwar said. That has importance for consumer goods as well as pharmaceuticals; since 2013, the European Union, for example, has prohibited cosmetics companies from testing products on animals.
The foundation for a printed organ is known as a scaffold, made of biodegradable materials. To provide nutrition for the organoid, microscopic channels only 50 microns in diameter — roughly half the size of a human hair — are included in the scaffold. Once completed, the “bioink,” a liquid combination of cells and hydrogel that turns into gelatin, is then printed onto the scaffold “like a layer cake,” Dr. Atala said.
Another important part of the process is constructing blood vessels as part of the printing. Pankaj Karande, an assistant professor of chemical and biological engineering at Rensselaer Polytechnic Institute, has been experimenting with skin printing since 2014 and recently had success in this step.
Using a cell known as a fibroblast, which helps with growth, along with collagen, as a scaffold, researchers at the institute printed the epidermis and dermis, the first two layers of skin. (The hypodermis is the third layer.) “It turns out the skin cells don’t mind being sheared,” Dr. Karande said, and they could ultimately survive.
But their work hit a snag: Without incorporating blood vessels, the skin eventually sloughs off. Collaborating with Jordan Pober and W. Mark Saltzman of Yale University, they eventually succeeded in constructing all three layers of human skin as well as vasculature, or blood vessels, which Dr. Karande said was essential to the skin’s surviving after it had been grafted.
The three began experimenting with integrating human endothelial cells, which line blood vessels, and human pericyte cells, which surround the endothelial cells, into the skin as it was printed. Eventually, after much trial and error, they were able to integrate the blood vessels with the skin and found that connections were formed between new and existing blood vessels.
The Coronavirus Outbreak ›
Frequently Asked Questions
Updated July 23, 2020
-
What is school going to look like in September?
- It is unlikely that many schools will return to a normal schedule this fall, requiring the grind of online learning, makeshift child care and stunted workdays to continue. California’s two largest public school districts — Los Angeles and San Diego — said on July 13, that instruction will be remote-only in the fall, citing concerns that surging coronavirus infections in their areas pose too dire a risk for students and teachers. Together, the two districts enroll some 825,000 students. They are the largest in the country so far to abandon plans for even a partial physical return to classrooms when they reopen in August. For other districts, the solution won’t be an all-or-nothing approach. Many systems, including the nation’s largest, New York City, are devising hybrid plans that involve spending some days in classrooms and other days online. There’s no national policy on this yet, so check with your municipal school system regularly to see what is happening in your community.
-
Is the coronavirus airborne?
- The coronavirus can stay aloft for hours in tiny droplets in stagnant air, infecting people as they inhale, mounting scientific evidence suggests. This risk is highest in crowded indoor spaces with poor ventilation, and may help explain super-spreading events reported in meatpacking plants, churches and restaurants. It’s unclear how often the virus is spread via these tiny droplets, or aerosols, compared with larger droplets that are expelled when a sick person coughs or sneezes, or transmitted through contact with contaminated surfaces, said Linsey Marr, an aerosol expert at Virginia Tech. Aerosols are released even when a person without symptoms exhales, talks or sings, according to Dr. Marr and more than 200 other experts, who have outlined the evidence in an open letter to the World Health Organization.
-
What are the symptoms of coronavirus?
-
What’s the best material for a mask?
-
Does asymptomatic transmission of Covid-19 happen?
- So far, the evidence seems to show it does. A widely cited paper published in April suggests that people are most infectious about two days before the onset of coronavirus symptoms and estimated that 44 percent of new infections were a result of transmission from people who were not yet showing symptoms. Recently, a top expert at the World Health Organization stated that transmission of the coronavirus by people who did not have symptoms was “very rare,” but she later walked back that statement.
While the work is preliminary — tested in mice — Dr. Karande said he was hopeful that the success in printing integrated skin and vasculature would set the stage for successful grafting in humans eventually.
The research, according to Dr. Karande, is painstaking and involves a lot of trial and error. “We have Plan A, which we often know won’t work and then we go down the list. We can often write about what works in five pages but have 5,000 pages of what didn’t work,” he added.
Dr. Gaharwar’s lab also is investigating whether human bone tissue can be printed for eventual transplantation. His hope, he says, is that in the future, patient radiographic scans can be translated into the exact shape needed for implantation, especially important in repairing craniofacial defects where the curvature needed can be difficult to recreate.
Like Dr. Gaharwar, Dr. Karande says that personalization is important. He says that his work has already shown that skin can be fabricated to match an individual’s color. And, because the skin is also critical in regulating body temperature, he is also working to engineer sweat glands into the skin, along with hair follicles.
“When we graft, we want to be able to recreate the full functionality of the skin,” Dr. Karande said. And by using the cells from a patient, rather than a donor, the risk of rejection is minimized or eliminated altogether.
Not surprisingly, researchers are also exploring the collection of data from testing. The team at Wake Forest is partnering with the technology company Oracle to capture the data from the organoids and analyze it with artificial intelligence. The project, known generally as the body-on-a-chip system, involves printing living tissue on a microchip to allow drugs to be studied for toxicity and efficacy even before clinical trials begin. The chips can be the size of a nickel or quarter, which is big enough to hold 10 to 12 miniature organs.
“We work a lot with researchers, pharmaceutical companies and biotech companies, and we are trying to seed advances as quickly as possible, analyze data and develop new drugs,” said Rebecca Laborde, the master principal scientist in Oracle’s health sciences division. “This is the most exciting project I’ve worked on in a long time.”
[ad_2]
Source link